It’s a scenario often seen by family members and care providers alike: A loved one receiving home health care begins to succumb to the difficult but oftentimes realities of aging.
Maybe they said they took their medication, but in reality forgot to.
Perhaps they say they’re feeling emotionally fine, but are actually depressed or lonely, not wanting to be a burden on those they know.
Or they could be angry, frustrated, and difficult to convince to adhere to the facets of their health care plan.
There is a fine line between supporting a loved one’s desire for independence and their need for different levels of supervision and monitoring, depending on their needs and conditions.
Remote Patient Monitoring (RPM) tools help immensely to provide a slate of detailed information in real time to healthcare clinicians, who are able to determine the current state of a patient and in some cases make a diagnosis remotely. The use of RPM and telehealth tools have come down from the large spike seen in their use in the early months of the pandemic but are still used nearly 40x more than before Feb. 2020, when their use was largely unknown.
With providers and clinicians seeing the benefits of this tech in a host of ways, its utilization is here to stay. In fact, by 2025, more than 70 million American patients will be using some form of RPM at least once per month.
But while the use of RPMs has become increasingly widespread, at the moment the lion’s share of physiological data that is monitored and communicated to clinicians does not extend much past the basics, as important as they are: blood pressure, heart rate, blood oxygen saturation, weight, and others. 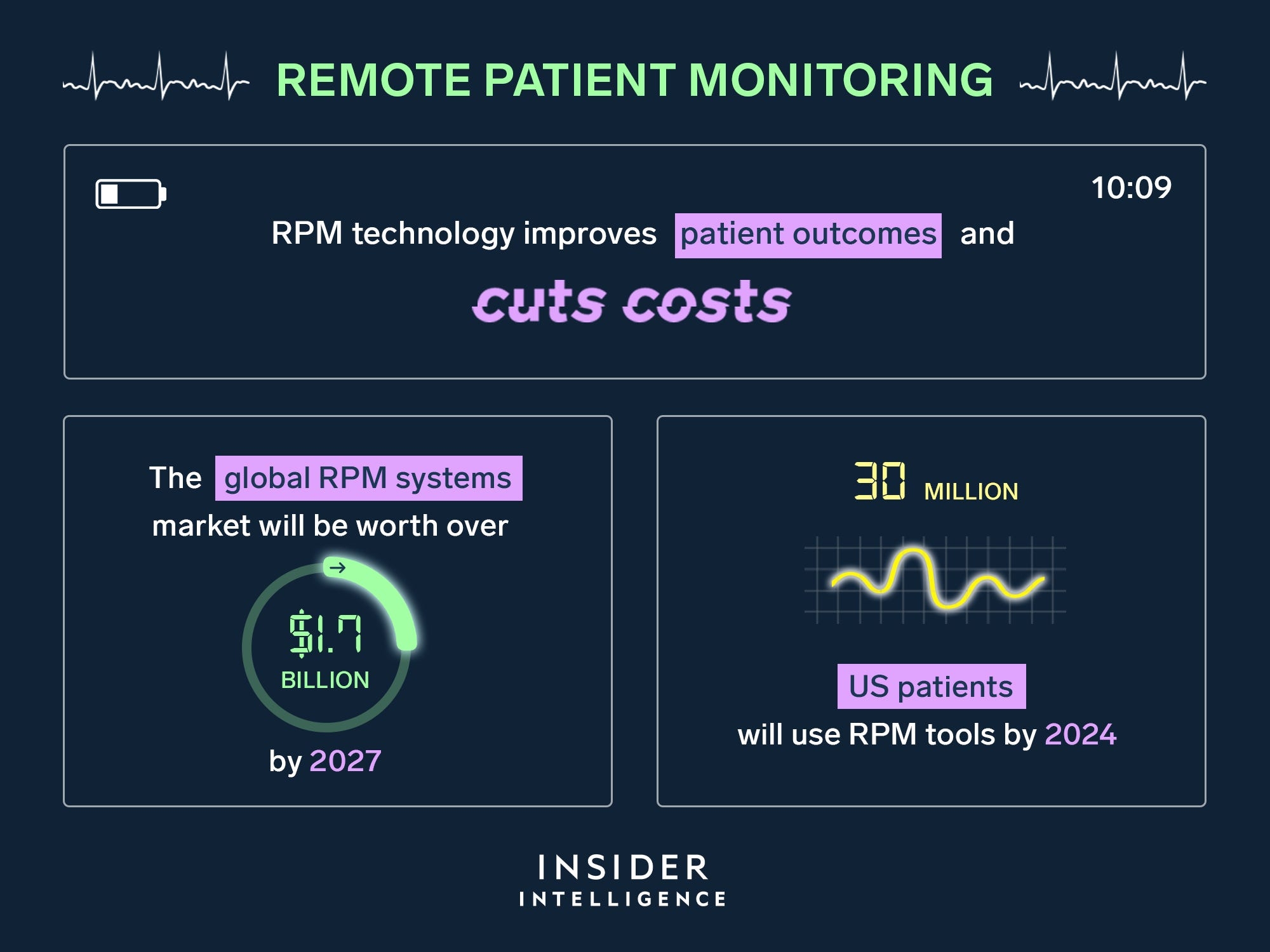
Photo credits: Insider Intelligence
However, several startups are developing RPM tech that is increasingly condition-specific, opening the door to a much fuller picture of the condition of patients dealing with chronic or potentially dangerous conditions.
A few examples include Palo Alto-based Spect, which developed a portable device that scans the eye for abnormalities and diseases, such as macular degeneration, glaucoma and diabetic retinopathy, all of which can lead to blindness. Data from the device is sent to proprietary software, which analyzes and sends the data to a patent’s clinician for further analysis.
Nearly 1 in 3 people over 65 have diabetes, and regular eye exams are critical to catching diseases in the early stages of development. However, many older Americans with a pre-existing condition – like diabetes – are not visiting their eye doctor as often as they should. Spect’s device, which can be used at home, makes the exam process easier.
Another startup, electronRx, has developed tech that uses algorithms to extract medical-grade vital signs and insights into cardiovascular and respiration function using smartphone sensors, with no additional hardware necessary. The tech streamlines RPM workloads while also lowering the cost of care, the company says.
Treating the Whole Person
But even the best tech tools can sometimes fall short where the treatment rubber meets the emotional road of a senior’s wellness journey.
With the average distance between a family member and a senior in the home being 270 miles, it simply isn’t feasible for a loved one to just pop by to check-in and dig deeper into issues. In addition, consistent physical visits from home care workers can become expensive, cutting into the cost savings seen from the use of RPM systems.
Another issue many seniors face is the loneliness that often creeps into their daily lives, which can potentially create serious detriments to their health.
Studies show that as many as 1 in 4 seniors experience social isolation, which only worsened during the pandemic. Additionally, many seniors are challenged with how to communicate their feelings and symptoms, what to look out for, and what is important information to share. Loved ones also can struggle with how to bridge the gap.
But more tech tools are coming online to address this issue, designed to treat the whole person, driving efficiencies, increasing outcomes, and including a sometimes overlooked but vitally important variable in a patient’s care plan – their family members.
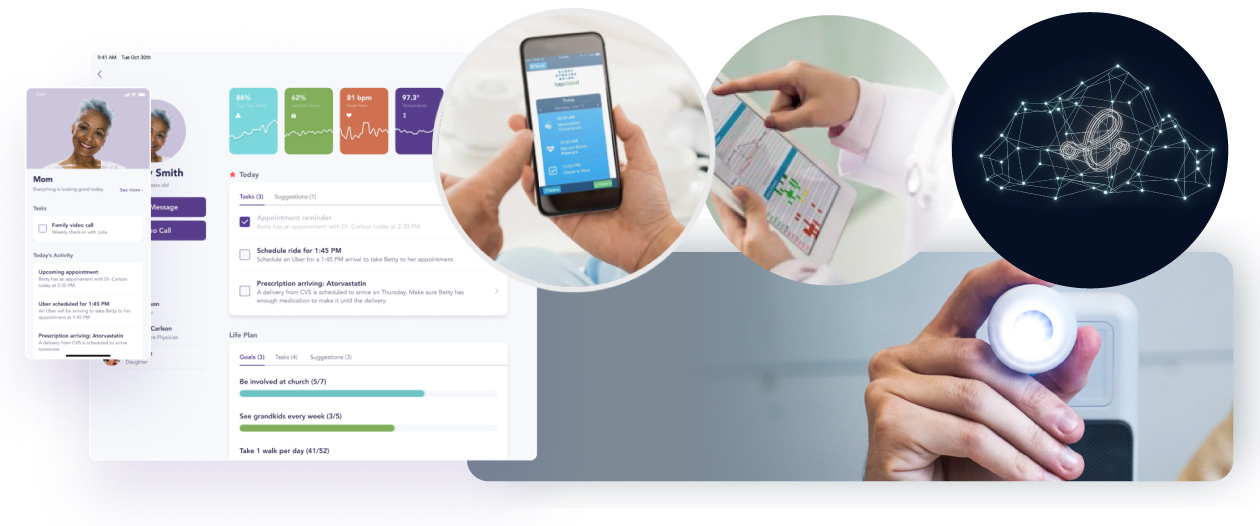
Chicago-based TapCloud, a Wellsky company, offers a cloud-based, AI-driven platform that allows patients to tap words on a smart device screen that indicates how they are feeling, with the words tailored to their specific physical and emotional conditions. The symptom tracker learns over time, helping drive need-based assistance as opposed to more expensive scheduled routine care, as well as supporting patient self-management.
The platform also wraps patients’ loved ones into the treatment mix, giving family members real-time insights into how they are doing. Family members can log into the platform and provide insights based on their deep knowledge and experience with a senior’s habits and personality, a critical component to effective treatment.
And although similar services that seek to treat the whole person are seen in the industry – like home care provider Lifespark’s “Lifespark COMPLETE” program – the implementation of such a treatment paradigm is still not widespread.
Intrepid USA Healthcare Services, the nation’s 12th largest home health care provider, utilizes TapCloud’s tech, and its CEO, John Kunysz says he’s seen the benefits.
“Someone can log in and determine that mom seems overly depressed, or seems lonely,” he said. “Family members should be involved in their loved one’s care, and these tools make that a lot easier.”
In the end, patient outcomes and satisfaction are bolstered by adding this remote family support, along with the intelligent, efficient administration of in-home services the AI component of the tech provides. Patients are kept out of the hospital more, while clinical efficiencies are increased.
“We use (tech tools) to look for differentials that show the degradation of a patient, but we can’t overlook the importance of a family member’s deep knowledge of a loved one who’s receiving care,” Kunysz said.
A patient’s social determinants of health need to be taken into consideration if they are to be treated holistically, and if anything, the inclusion of family members into a patient’s treatment plan attends to at least some of those core principles. A senior who knows their family is close by – even if it’s virtually – and is as involved in their treatment plan as their clinicians, is more apt to follow protocols, feel less isolated, and in the end, be healthier as a result.
Posted by
Join us!
The retreat for home health care and hospice leaders innovators.
May 17-19, 2026 | Palm Springs, CA




-2.png)

-2.png)


Comments