From his past roles as CTO at the U.S. Dept. of Health and Human Services, Secretary of the Louisiana Dept. of Health and Hospitals, and Managing Director of Microsoft’s Worldwide Health initiative, Bruce Greenstein has been around enough to know the inside baseball of the industry.
Now, after almost five years as EVP and Chief Strategy & Innovation Officer at LHC Group, one of the nation's largest home health care providers, Greenstein once again finds himself at a new phase in his career.
The ink is dry on home health care giant Optum’s (a subsidiary of UnitedHealth Group) acquisition of LHC, a $5.4B deal that turned heads when it closed earlier this year. Although full integration of LHC into Optum will take some time, Greenstein will undoubtedly help transform operations with the innovative know-how he’s honed in both the public and private health care sectors.
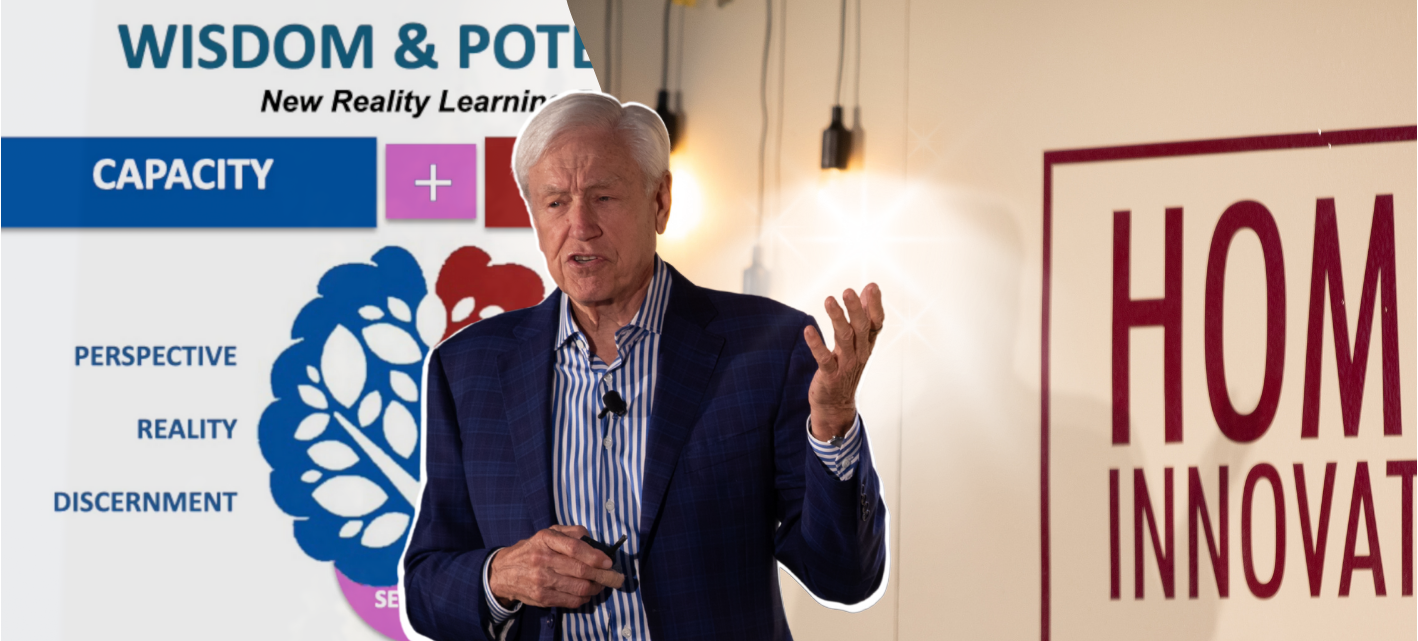
A featured speaker at the upcoming Home Care Innovation Forum, we chatted with him about where he sees the trajectory of M&A activity heading, what he thinks home health care might look like by the end of the decade, and whether small regional operators will become a thing of the past.
This transcript has been edited for length and clarity.
“The Issues with Conveners and How to Protect your Bottom Line” is the title of the talk you’re planning. What are some key points you’ll make?
Greenstein: One: It's not just about rates. Two: It's about how you structure the payments, which has to do with a case rate, an episode of care, or some single payment for multiple visits. In other words, moving away from just a pure pay-for-visit methodology. Value has to be part of the equation. We can't run away from it. You need to think about re-admission rates. All those pieces come into play.
Now, here's the problem. The providers that can negotiate a deal like this and then deliver that quality of care is much different than why many conveners are in business, which is to get the lowlifes out of the system – those with no integrity, that abuse the process. They over-treat patients and conveners don't tend to come in with very sophisticated fraud and abuse detection capabilities. There is going to be some sorting out process and conveners have to be vigilant rather than just trying to go with one blanket policy of, say, five visits for every patient. We've got to go ahead and sift that out.
If you're a new convener in the home health market, you'll want to find the providers you'll refer to all the time in your first round, maybe the first three rounds. You'll need an algorithm to figure out who gets what referrals. You're going to have a different set of requirements, whether it's around documentation, how often you require a new authorization for additional visits, or for another episode of care.
Those have to be carefully put together, which will require data exchanges. To some working on this right now, both conveners and data partners, it's going to mean a higher level of sophistication. I think that's the direction that the industry has to move towards. If you're a smaller provider and want to swim with the big dogs, then you just have to up your game and be able to be in that crowd. You must be able to deliver those quality outcomes to measure them the right way and negotiate for a different payment arrangement.
Optum’s purchase of LHC Group made a lot of news. What will your role be after the full integration?
Greenstein: Full integration will take a while, and people who know me know I'm willing to be as open as possible. We just don't have any answers about whether my role will be different. So, right now, it's Chief Strategy Officer. We’re trying to make this integration seamless from an operations perspective. Optum is an incredibly large and complex organization. United Healthcare (which Optum is a part of) is the fifth largest company in America. There may be 20 years of opportunity for me to connect care in the home with all these other parts of the company.
By June, I'll have a better idea of what the top three to five priorities look like. The one thing that Optum is clear about is you have to hit your numbers. After that, then you figure out how to plug in with the organization, but all of the integration pieces are secondary to hitting the numbers that we've committed to.
What that really means is that we can't change our business model, and we can't try to morph our company into something different. We have to deliver on what we committed to when we sold the company, which should be reassuring to many people.
Where do you see the current trajectory of M&A in the industry heading? Are small regional operations a thing of the past?
Greenstein: I don't think they’ll become something of the past. I think the smaller companies have figured out how to keep their overall cost of providing care and running the company to be very low. They can be a lot more flexible. And so they can take payers that larger platform companies that have several costs like sales, legal, and compliance have a harder time taking. MA payers and small mom-and-pops figured this out a while ago. They’re able to make margin on lower-paying payers, and even though maybe they'll merge a little bit, these providers will continue well into the future.
I do think there will be more M&A activity. We've not seen the end of consolidation from the big players. I think that if you look at some of the larger assets that are owned by private equity – for three, four, five years – when that five-year itch hits the reality is to figure out how to exit. So keep your eye on those.
There will be pressure from seeing another potential Medicare rate reduction, and at the same time, the rise of value-based care. So if you're just trying to eek things out without changing, with the current market conditions, you're going to be one that's likely to be sold. And if you're a weak provider, another round of rate cuts will make you teeter on insolvency and you'll look like a good target (for acquisition).
Some in the industry view conveners unfavorably, but they are not entirely negative; in fact, some believe they fulfill a crucial function.
Greenstein: We looked at providers in Los Angeles County. First of all, there are hundreds and hundreds of providers there. But their average length of stay is almost 200% of the rest of the country. The amount that gets filled by Medicare fee for service is something like three times the amount seen nationally. Maybe there are more difficult patients in Los Angeles, maybe they have other social determinants of health challenges…or maybe there's a whole load of crooked providers just milking the system?
If I were running a health plan there, I would definitely drop in a convener to go ahead and comb out the waste and the abuse that's taking place there. At the moment, CMS doesn't do a lot of focused activities on home health for fraud abuse. We definitely did when I was working for Tom Scully in the ‘90s. We cracked down on the home health industry and it was rife with fraud and abuse, and now, most of the industry is full of integrity. If you're a convener, there's definitely a purpose (for you) in some parts of the country more than others.
Examining the trends, by 2030, what transformations will have occurred in home health care, and what aspects will have remained the same?
Greenstein: Medicare Advantage will be the overwhelming majority of the Medicare program, and Medicare Advantage doesn't just want to buy a discounted version of the Medicare fee-for-service benefit. They want something different and the clinical processes are different. The workflow and communications will be different.
The provider will be acting on behalf of member services for the health plan and they have a lot they can do while they're in the home. It's no longer good enough to just do an OASIS, some treatment, and teaching and training. It has to change.
There's a Steve Jobs moment for home health right now, which is: “My customers don't know what they want until I show them.” Right now, Medicare Advantage is not schooled in the understanding of this. I'm seeing it firsthand now that I'm owned by the largest health plan in the world. There's a lot that we can teach health plans and it can be creative on all sides: The patient, the payer, and the provider.
Posted by
Join us!
The retreat for home health care and hospice leaders innovators.
May 17-19, 2026 | Palm Springs, CA




-2.png)

-2.png)


Comments